Intellectual property
INGO opposes vaccine patents

In the beginning of the Covid-19 pandemic, a frequently heard comment was that the virus knows no borders and we are all in this together. Very soon, though, it became clear that the impact of the virus, if not the virus itself, does indeed differ between rich and poor regions. People of colour and those in the global South are much more likely to be infected and die from Covid-19, and are much more vulnerable to the economic fall-out of the pandemic.
Adding to those disparities is the unfair way that life-saving vaccines are being priced and delivered in different regions of the world. Distribution is far from equitable. According to the Financial Times, African countries had only received 40 million vaccine doses for 1.2 billion people by mid-May. Some of the poorest countries have not yet even begun to immunise their populations.
Vaccine deliveries in low-income countries have recently started, thanks to the efforts of COVAX (the Covid-19 Vaccines Global Access, a global initiative aimed at fair distribution of Covid-19 vaccines, led by the World Health Organization). Yet COVAX itself says distribution will fall short because of a shortage. Only three percent of people in poor countries can hope to be vaccinated by mid-year and only one fifth at best by the end of 2021.
There are two major reasons for this dim outlook, and both stem from the world’s dependence on a handful of pharma giants to produce vaccines.
The first reason is that these companies simply can’t make enough vaccines for the entire world on their own. Yet they refuse to share their science and technology freely with other qualified manufacturers that could help in the effort.
The second reason is that pharma companies, through their patents, have monopolies on the sale of these vaccines, which in turn gives them powers to set prices. Particularly in a scarcity situation, having these rights means a patent owner can set whatever price it wants for a product in demand.
While some price negotiations with buyers and public agencies do take place, patent owners control crucial information on product development costs, which is essential to setting the price. This information is part of the companies’ intellectual property; they are not required to disclose it. Such an imbalance inevitably disadvantages those with the least amount of information, leading to higher than necessary prices in poor countries (see box).
As many examples show, poor countries sometimes pay more than they should for vaccines. This disadvantage is in addition to the disproportionate damage they already suffer from the pandemic itself. Oxfam’s recent report “The inequality virus” shows how precarious their situation is (see Sabine Balk in D+C/E+Z e-Paper 2021/03, Monitor section). The pandemic has put a strain on low income countries’ external resources, with a 20 % fall in remittances, a 25 % fall in foreign direct investment and sharply increased capital flight.
Pausing patent protection
The response from the Group of 20 leading economies has so far been inadequate. Creditor nations have delayed debt service payments for only 1.66 % of the debt owed by poor countries. Immediate debt relief across the board, including from banks and investment funds, is urgently needed. So too is action to increase vaccine supply and bring prices down to affordable levels.
Several solutions have been proposed, but they are being blocked by rich countries and pharma companies. For example, a UN initiative called the “Covid Technology Access Pool” calls on pharma companies to voluntarily disclose their vaccine technology to other producers so that more vaccines can be made. So far, none of the big pharma companies has done so.
Similarly, some rich countries say they’ll donate some of their vaccine surplus to poor countries. This is helpful. But donations of unknown amounts at unspecified times is an inadequate solution and will not bring enough vaccines to countries that need them.
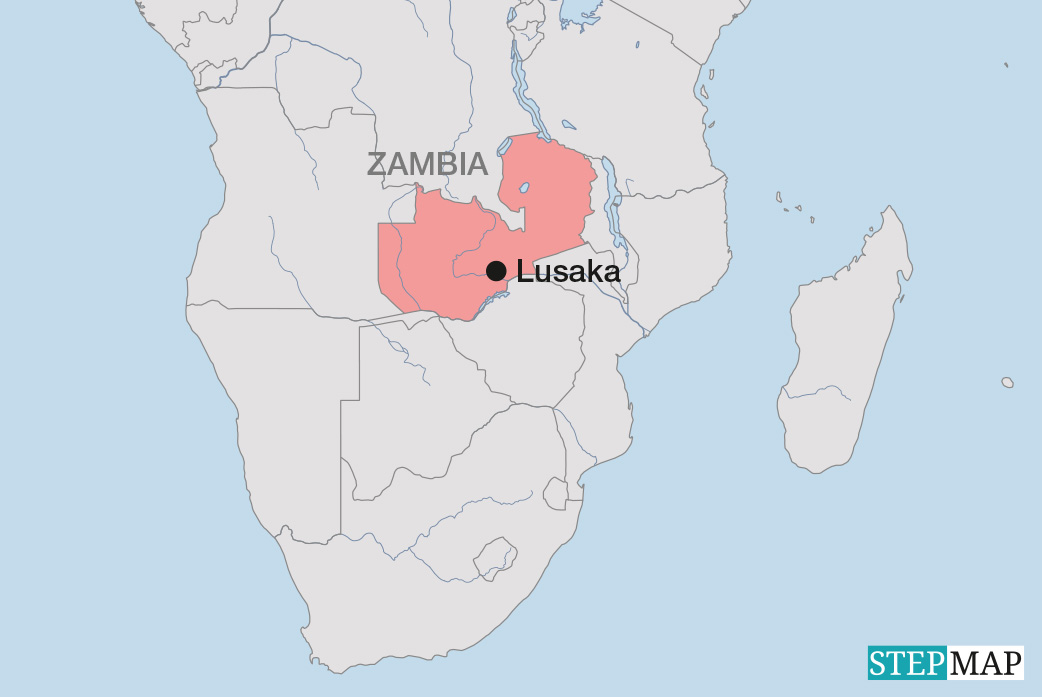
The reform that would help the most would be to pause the patent protections given to pharma companies until the world reaches herd immunity against Covid-19. South Africa and India, supported by 100 developing countries, are calling on the World Trade Organization (WTO) to do this. Civil-society organisations endorse this proposal. However, rich nations, led by the US, UK, EU and Japan have opposed this proposal, although the Biden administration in the US has changed its stance, with several other governments following suit.
In an open letter to President Biden, 175 individuals including former heads of state and government and Nobel laureates call on him to back a temporary waiver of patent protections. The letter was organised by the People’s Vaccine Alliance, a coalition of health and humanitarian groups.
Pharma companies argue that keeping their patent protections is the best way to guarantee innovation and thereby maximise the benefits for humanity. In fact, though, the patent system locks away the benefits of publicly funded science and thus delays the end of the crisis. Vaccines are public goods paid for by over $ 100 billion of taxpayers’ money. These technologies should be freely available in the interest of protecting public health.
Some pharma companies also contend that pausing patent protections would allow sub-standard vaccines to enter the market. But pharma firms worldwide already produce a wide range of medicines and vaccines under licence with good results. They are fully capable of producing a Covid-19 vaccine that meets strict WHO standards – if they are allowed to do so. Suggesting otherwise is a long-used tactic of pharma companies to protect their profits.
Ultimately, since the coronavirus indeed does not recognise borders, ensuring an adequate and affordable supply of Covid-19 vaccines in poor countries will protect public health worldwide. Monopolies on vaccine technology stand in the way of scaling-up production and reducing prices. Expanding production and reducing prices in developing countries would contribute to the global public interest, both in the current pandemic and in future ones.
Marion Lieser is executive director of Oxfam Germany.
mlieser@oxfam.de