Sustainable development
Bengali doctor says pandemic proved validity of SDG agenda

In the summer of 2021, international media ran many stories about the devastating Covid-19 wave in India. Was Bangladesh affected in the same way?
Well, our country was hit by the pandemic, but we were not overwhelmed in the sense of dead bodies drifting in our rivers, as was apparently the case in India. In Bangladesh, charitable organisations ensured that the deceased were buried properly. When the pandemic started in 2020, we certainly felt overwhelmed, but that was largely mental. We were not sure how we would cope. Looking back, I would say that we had serious difficulties, but did not suffer a disaster.
What pandemic impacts do the poor communities feel?
The pandemic affected all communities, including the middle classes and lower-middle classes. Everyone was at risk of infection, many people did fall ill, some had to be hospitalised and some even died. However, the economic impacts hit poor people stronger. For example, all domestic helpers lost their jobs. Their employers told them to stay at home instead of coming to work because they did not want to have an outside person in their households in order to contain infection risks. Markets stayed closed, small business stopped working and transport services were drastically reduced. Even garments production stalled briefly (see Nazma Akter on www.dandc.eu). As a result, many people with low and moderate incomes temporarily lost their livelihoods, and that caused considerable pain.
Did it lead to hunger?
Many families certainly only had two meals per day instead of the three meals they are used to, but Bangladesh did not see a serious hunger crisis. In times of need, community members support one another in our country. Civil-society organisations, including ourselves, delivered food to vulnerable people, and the government adopted selective support policies for the poorest communities. Civil society, the private sector and state agencies cooperated well. That said, more people than is normally the case probably did not get sufficient amounts of vitamins and proteins. Things have been going back to normal however.
Bangladesh used to be one of the world’s poorest countries, but after three decades of fast economic growth, it is now a lower-middle income country. Would the impacts of Covid-19 have been worse if the pandemic had started in 1990 rather than in 2020?
Yes, definitely. On the other hand, our country keeps developing, so we would prove even more resilient should a similar disease emerge in 2030. Many social indicators have improved, including average incomes, literacy and life expectancy. Compared with other South Asian countries, our data regarding child and maternal mortality are very good too.
The country’s birth rate has been close to the replacement rate for quite some time, so our population is not growing anymore (see Najma Rizvi on www.dandc.eu).
Our infrastructure has improved, and that includes health care. All this adds up to Bangladeshis’ average health status being better today than it was 30 years ago. Therefore, we are obviously in a better position to cope with any new health challenge.
In many countries, health systems were overwhelmed. For example, there were so many Covid-19 patients in intensive care, that there were no beds left for other patients. Important operations had to be postponed. Moreover, some patients shied away from going to clinics because they feared they might be infected there.
We obviously had those problems in Bangladesh too. Indeed, many private-sector health facilities closed for some time to avoid infection risks. Coronavirus is a global phenomenon, and it definitely caused hardship here. My point is that things did not turn out as bad as we initially feared. Among other things, we found that mobile telephones were very useful, with many people asking for – and getting – medical advice without going to health centres. In Bangladesh, almost everyone has a mobile phone today. Increased literacy rates helped too, because many people today access information on the internet. Generally speaking, the development achieved in the past decades has proved useful in this health crisis.
How do you assess long Covid?
That is hard to say. Much research still needs to be done internationally, and we hope to benefit from such information. I have had three Covid infections myself, and I now experience a kind of mild cramp that I did not have before.
Are those cramps a consequence of coronavirus?
I do not know. Eventually, clinical research will provide information. As a matter of fact, many people may be experiencing similar or other symptoms, but they do not inform us. In a developing country like Bangladesh, people will tolerate symptoms that do not really disable them without going to the doctor. Some poor people do not try to access medical care at all, given that they lack money to pay for services. To get a full picture of all Covid-related symptoms, we will need international studies.
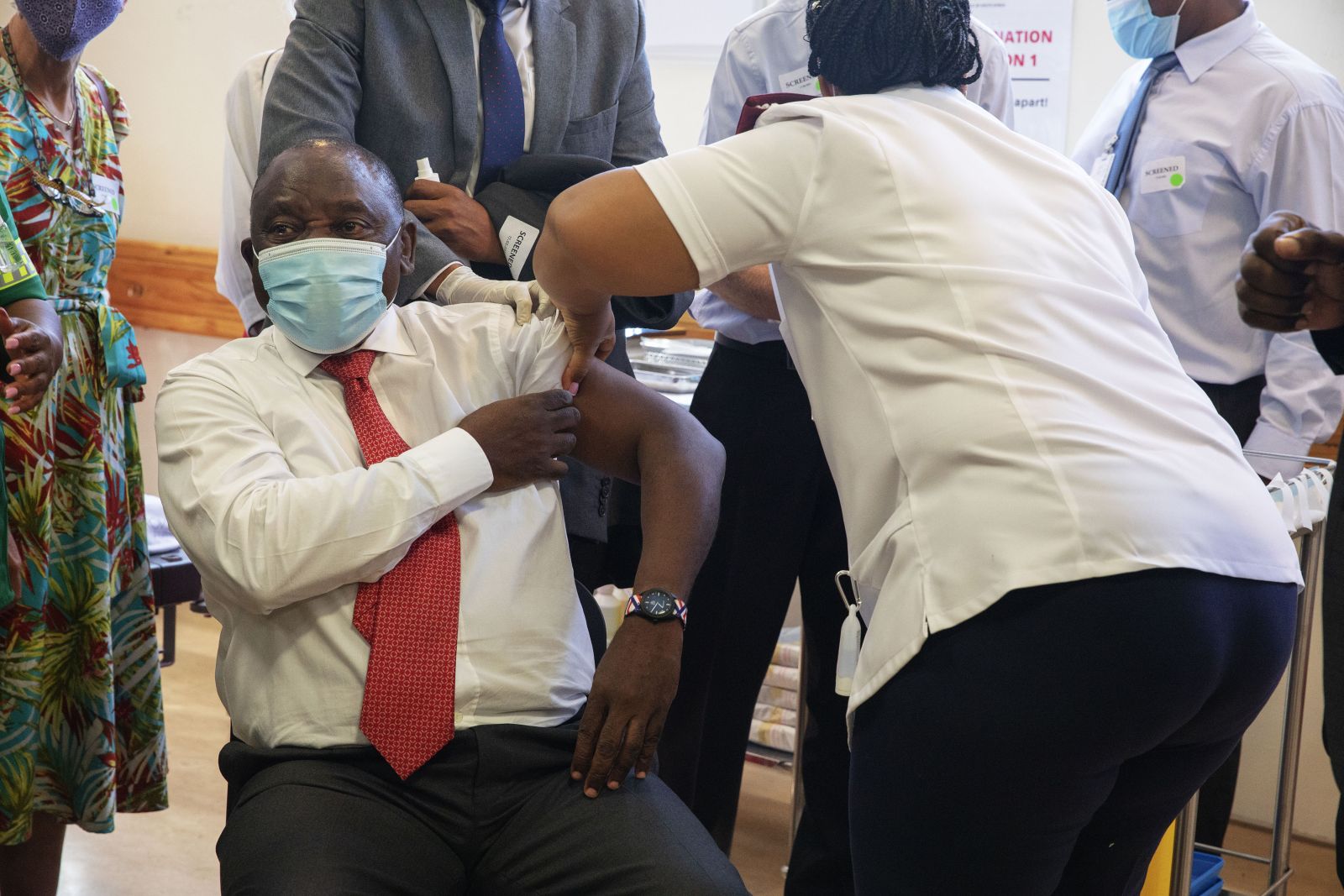
How did the vaccination campaign go?
Well, we basically used two vaccines. The one developed by Oxford University and a Chinese one. We made good progress, but would have achieved more in shorter time if we had been allowed to manufacture a vaccine in Bangladesh. We have the industrial capacity. Oxford University prominently cooperated with AstraZeneca, the pharma multinational, but it also made an agreement with an Indian company. In return for the production license, the company promised to distribute the vaccine to developing countries in a cost-covering non-profit approach. But India stopped exporting that vaccine when its death toll started to rise fast last year. Luckily, we could rely on the Chinese vaccine at that point. Bangladeshi facilities could have produced either vaccine, and that would have reduced costs. That did not happen.
The innovative mRNA vaccines of Pfizer/BioNTech and Moderna are considered to be more effective, but they also require better infrastructure, especially in regard to cold chains. Would it have made sense to manufacture them in your country?
Yes, of course. In our urban areas, we have the capacity to keep medical supplies cold, though I’ll admit it can be quite difficult in rural areas. One lesson for Bangladesh certainly is that we must keep improving the capacities of our pharma sector. So far, only one vaccine is under research in our country. We need more research and must become able to create innovative pharmaceuticals ourselves. We can – and will – get there.
Looking back, what kind of international support does Bangladesh need in a global pandemic?
- First of all, we need information. Unless we know what is going on in other countries, we cannot prepare for what may happen here. Honest and comprehensive information is essential. Without it, we cannot adopt evidence-based policies.
- Technology transfer matters too, though our pharma industries have become so strong that in many cases the license to use intellectual property rights will do.
- There is no denying that we also need funding.
- Finally, international supply chains must be kept viable to the extent possible. Our people suffer when imports and exports become restricted.
Is there any general lesson policymakers should learn from the pandemic?
I think that Covid-19 showed us once again that we need a holistic understanding of development. Economic growth in itself is not enough. It must be used to improve infrastructure, including in the health and education sectors. Better infrastructure makes communities more resilient, and it will ultimately reinforce economic growth. These things are interrelated. In this sense, the pandemic actually proved that the Sustainable Development Goals add up to a convincing agenda.
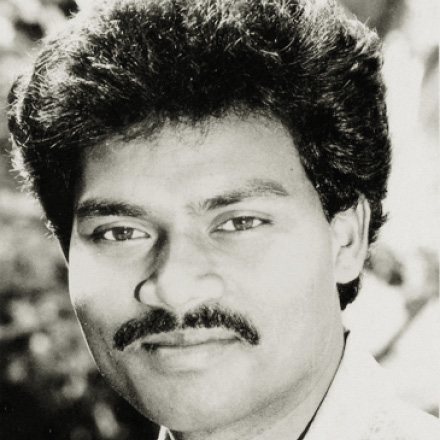
Manzur Kadir Ahmed is a medical doctor and the chief executive of Gonoshasthaya Kendra (GK), a non-governmental organisation focused on health care.
Gonoshasthaya Kendra (GK):
https://gonoshasthayakendra.com/