Women's health
Dangerous for mothers and babies
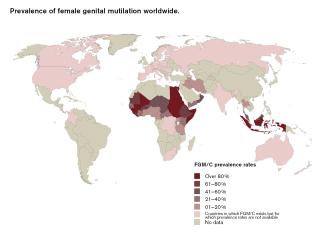
About 200 million girls and women worldwide have been cut. FGM is widespread in 29 African countries, and in over ten of them, at least half of all women have been cut. The practice is also common in Southeast Asia, especially in Indonesia, and in the Middle East. Due to migration, FGM is also prevalent in Europe, the USA, Canada and Australia.
The World Health Organization (WHO) has identified four major types of FGM. The most invasive procedure is type III, also known as infibulation. It involves narrowing the vaginal opening through the creation of a covering seal, formed by cutting and repositioning the labia minora and/or labia majora, with or without the removal of the clitoris. The wound is stitched closed, leaving only a very small opening to allow for urination and menstruation.
FGM is most often performed on children between infancy and the age of 14. During and immediately after the procedure, complications such as excessive bleeding, severe pain, shock and wound infections usually occur. These eventually leads to long-term consequences like chronic pain, fistulas, urinary and menstrual problems, incontinence, sexual problems, complications relating to the scar tissue, keloids and trauma.
Infibulation also involves de-infibulation and re-infibulation procedures. De-infibulation is the surgical procedure to open up the closed vagina. This is often performed several times, for example on the wedding night to allow for sexual intercourse and prior to childbirth. Re-infibulation (reclosing the vagina) usually takes place after each childbirth. These processes pose serious consequences for both the mother and the unborn child.
The formation of scar tissue prevents the birth canal from expanding the way it should. As a result, deliveries often last longer than normal, with a greater risk of complications. The scar tissue can tear, which in turn causes tearing in the blood vessels, nerves and muscles of the pelvic floor. Tears that extend into the anal canal are common as well and may result in fistulas and incontinence.
Infibulation also makes birth riskier for babies. Drawn-out deliveries can dangerously limit oxygen levels, causing injury or even death. Tears and wounds in the mother’s tissues also make it much more likely that she will transmit HIV/AIDS to the baby. Due to the fact that women may bleed to death during childbirth, many are forced to undertake a caesarean section. In general, childbirth injuries are significantly worse among women who have undergone FGM (particularly type III), thereby increasing the risk of maternal and infant mortality.
Terre des Femmes, a human-rights organisation for women, has been engaged since 1981 in the prevention and cessation of FGM. Since 2016, TDF has been coordinating the EU-funded CHANGE Plus project, training African diaspora communities within the EU to contribute to the abandonment of FGM within their own communities. Sensitisation and awareness-raising are crucial measures.
Doctors, especially gynaecologists, midwives and nurses play a central role in advising, educating and treating women and girls who have been affected by FGM. These professionals are also very likely to encounter survivors of FGM or girls at risk. TDF thus offers training for medical professionals for the purposes of education, prevention and treatment of affected women and those who are at risk.
Since the priority is child protection and support for survivors, awareness must be raised in ways that are respectful, thoughtful, flexible, constructive and well informed.
Idah Nabateregga is head of the department of female genital mutilation at Terre des Femmes.
fgm@frauenrechte.de
Links
Terre des Femmes:
http://www.frauenrechte.de/online/index.php/en/home-engl
CHANGE Plus Projekt:
http://www.change-agent.eu