Sexually transmitted disease
HIV/AIDS still haunts South Africa

South Africa’s HIV/AIDS scenario began to improve with the arrival of ARV treatment from 2004 on. The situation remains serious, nonetheless. Today, about one in seven South Africans are living with HIV. That is the highest rate internationally, but down from about not quite one in five. A bit less than two thirds of the infected persons now get the ARV treatment that prevents the virus from triggering the dangerous immune deficiency. Patients who take the drug regularly, can live rather normal lives.
Recent research shows that the infection rate among people over 40 is one in four and thus above average (Mann-Goehler et al., 2024). About 37 % of them are not on ARV medication. Unsurprisingly, the figures tend to be particularly bad in rural areas, where poverty is wide-spread, where education levels are often poor and traditional norms quite strong.
The research data flesh out two connected issues, says Wade Ngoza, a doctor at Pretoria’s Mamelodi Regional Hospital. The good news is that 63 % of the elderly patients are indeed getting the required healthcare. Ngoza also appreciates that the rates of HIV infections have decreased across the country, that more people know their status and that ARV uptake is holding up well.
On the downside, far too many patients are still not getting what they need, and elderly persons are more likely to be HIV positive. Moreover, Ngoza worries that there may be many unrecorded cases: “We don’t know the number of seniors who are living with HIV unknowingly and untested.” He does not want to see those seniors being left behind any longer.
A strong focus on the young is actually a long-standing pattern in South Africa. ARV treatment first became available free of charge in 2004. Initially, it was offered exclusively to people under the age of 40. At that time, this age cohort was also the target group for treatment messaging and HIV prevention campaigns.
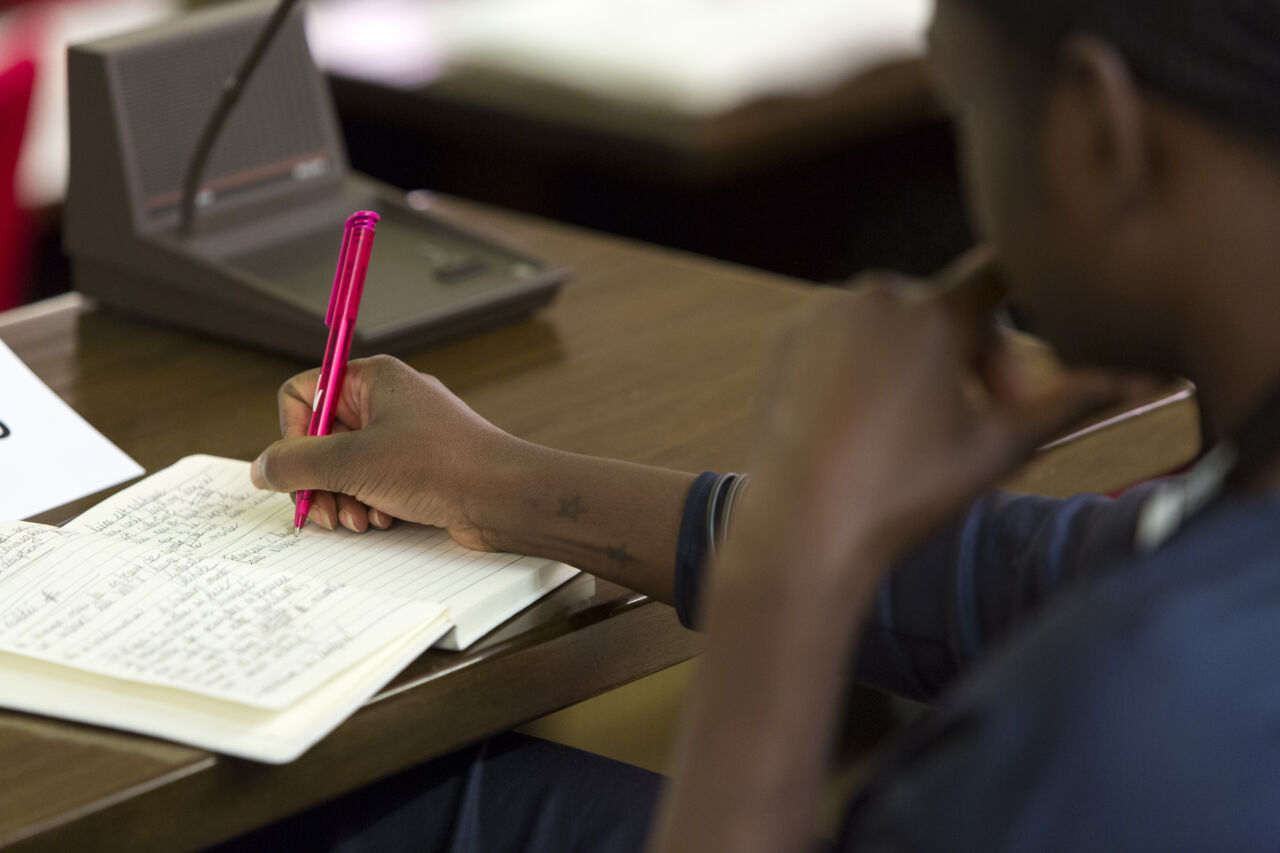
The idea was that the young are the sexually most active. “Via music gigs, billboards, newspaper adverts, festivals, drama plays, HIV was messaged narrowly as a danger to young South Africans,” remembers Bromley Naka, a social worker. The government expected that transmission in other demographics would stop if HIV could be eliminated in the age group 14 to 24. It was simply assumed that seniors do not engage in risky sexual behaviour or take drugs.
UNAIDS data show that persons aged 14 to 24 are indeed most at risk, accounting for about 30 % of all new infections in South Africa in 2017. The implication, however, is that 70 % of new infections affect other people. They obviously matter very much.
Age-related stigma
The belief that older people lived by higher moral standards was always wrong, says Naka. One side effect of this belief was that the stigma of infection became worse with age. The social worker reports that, out of shame, many seniors did not show up and “died needlessly in their homes.”
Naka says that he knows several cases of seniors who say they were abandoned by their children when their HIV infections became known and began to get worse. Loneliness thus made the suffering worse.
Communities had a tendency to hush up things. Welele Sikhosana, a 63-year-old pastor and HIV activist, recalls: “At funerals of seniors, preachers were lying that the cause of death was malaria when we knew our elderly friends were dying of untreated HIV.” He adds that it was morally embarrassing for a 65-year-old grandmother to tell her children and grandkids that she needed ARV drugs because of a new HIV infection. The family would have considered her to be a moral failure. “We were living a lie,” Sikhosana concludes.
A former sex-worker’s activism
Thembi Malaika (name changed) probably got her HIV infection in her late 40s or early 50s. The retired sex worker is now 70 and lives in Johannesburg. She says that HIV programmes “badly failed the elderly from the start.” Not least, people who earned their living with prostitution, as she did, were obviously at risk, and not all of them were young.
Malaika says she has helped 33 seniors over the age of 59 to disclose their HIV positive status to their families.
She is proud to have contributed to making the culture change slowly. “It was an uphill struggle,” she recalls. “We were dying, came out and confronted the government.” Today, billboards and TV advertising feature elderly citizens speaking about their infections and encouraging everyone to get tested and enrol for health insurance.
Though things eventually began to improve, stigma persists. When someone in their 70s gets an HIV test, they are likely to hear disparaging remarks from healthcare staff. Moreover, Malaika knows 70-year-old persons “who are taking ARVs secretly”. They fear their grandchildren will reject them if they learn the truth.
Side effects of poverty
Poverty matters very much too. Brenda Wandiswa works as a welfare manager for the government of Gauteng, the country’s wealthiest province. She points out that seniors have some of the nation’s worst rates of hunger, joblessness and homelessness. In 2019, 30 % of the elderly population were estimated to lack food security. According to news reports, some senior citizens quietly starve to death in their rural cabins in Eastern Cape, the poorest province.
Such problems tend to be worst for senior citizens who are not 61 yet. At 61, they become eligible for a small government pension, starting at the equivalent of $ 60 per month. Those who lack that kind of support, but are unable to earn a livelihood, find it particularly difficult to adhere stringently to an ARV regimen. Anyone who must improvise from day to day will always struggle to stick to a routine. While the medication is available free of charge, a trip to a clinic may prove unaffordable, especially in rural areas.
ARV treatment should not be derailed by ageism, stigma and moral judgement. South Africa has made progress, but as Wandiswa can confirm, it is not there yet.
Reference
Mann-Goehler, J., et al., 2024: HIV among older South Africans in rural areas.
https://theconversation.com/hiv-among-older-south-africans-in-rural-areas-big-study-shows-theres-a-problem-thats-being-neglected-222954
Michael Moyo is an African journalist who does not want this contribution to be published under his name because his professional situation has changed since he accepted the assignment to write this story.
euz.editor@dandc.eu